Prevalence Of Alloimmunization To Red Cell Antigens Among Multiply Transfused Patients With Sickle Cell Disease In Kaduna, Nigeria
DOI:
https://doi.org/10.60787/njhaem-7-1-2-68Keywords:
Total Life Time Transfusion, Sickle Cell Disease, Multiple Transfusion, Red cell AlloimmunisationAbstract
Introduction: Red cell transfusion is an important modality in the treatment of complications in patients with Sickle cell disease (SCD) or Thalassaemia. However, this is associated with alloimmunization, resulting in destruction and immune-mediated clearance of the destroyed RBCs. Alloimmunization to RBC antigens complicate RBC crossmatching and delays the process of providing compatible blood for transfusion.
Aim: To determine the prevalence and pattern of alloimmunization in Multiply Transfused patients with SCD in Kaduna state.
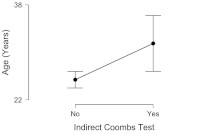
Methods: A cross-sectional descriptive study of One hundred and thirty-one (131) individuals with SCD who had received 10 or more units of packed cells transfusions. Total Lifetime Transfusion (TLT) was defined as the total number of blood units received over a whole lifetime. Red cells were typed for ABO and Rh blood groups and Indirect antiglobulin test (IAT) for antibody screening using the saline spin tube technique and identification was done with the 3 cell Maxiscreen and 10 cell identification panel. Results were analysed using Jeffrey’s Amazing Statistical Programme (JASP) version 0.14.1, Dec 2020, statistical software.
Results: The prevalence of red cell alloimmunization was 15.3% while the risk of alloimmunization per unit of blood transfused was 1.2%. Ten (10) types of alloantibodies were identified and Anti-Lea was the most frequently occurring antibody (3%).
Conclusion: There is a high prevalence of alloimmunization among patients with SCD. Therefore, multiply transfused individuals should undergo screening for the most commonly occurring clinically significant antibodies.
Downloads
References
Howard J. Sickle Cell Disease: when and how to transfuse. NCBI/PMC. 2016;1:625–31.
Chou ST. Transfusion therapy for sickle cell disease: a balancing act. Hematology Am Soc Hematol Educ Program. 2013;1:439–46.
Contreras M, Allard S. Clinical Blood Transfusion. In: Postgraduate Haematology. 7th ed. Wiley Blackwel; 2016: 214–245.
Inati A, Mansour AG, Sabbouh T, Amhez G, Hachem A, Abbas HA. Transfusion therapy in children with sickle cell disease. J Pediatr Hematol Oncol. 2017;39(2):126–32.
Adewoyin S. Erythrocyte Transfusion and Alloimmunisation Patterns among Sickle Cell Disease Patients, Benin City, Nigeria. Br J Med Med Res. 2016;11(10):1–8.
Kosaryan M, Mahdavi MR, Roshan P, Hojjati MT. Prevalence of alloimmunisation in patients with beta thalassaemia major. Blood Transfus. 2012;10(3):396–7.
Rashmi Sood, RN Makroo, Vimarsh Riana NR. Detection of alloimmunization to ensure safer transfusion practice. Asian J Transfus Sci. 2013;7(2):135–9.
Rosse WF, Gallagher D, Kinney TR, Castro O, Dosik H, Moohr J, et al. Transfusion and alloimmunization in sickle cell disease. Blood. 1990;76(7):1431–7.
Onyebuchi C, Khaliru A, Akinyanju Olu. National Guideline for the Control and Management of Sickle Cell Disease. 2014;1–2. Available from: http://scsn.com.ng/wp-content/uploads/2014/11. Accessed 3pm, 4 Feb 2020.
Kangiwa U, Ibegbulam O, Ocheni S, Madu A, Mohammed N. Pattern and prevelence of alloimmunization in multiply transfused patients with sickle cell disease in Nigeria. Biomark Res. 2015;3(1):15–22.
Obi EI, Pughikumo CO, Oko-Jaja RI. Red blood cell alloimmunization in multi-transfused patients with chronic kidney disease in Port Harcourt, South-South Nigeria. Afr Health Sci. 2018;18(4):979–87.
Patel J, Shukla R, Gupte S. Red cell alloimmunization in multitransfused patients and multiparous women. Indian J Hematol Blood Transfus. 2009;25(2):49–52.
Corrine Jury, Yutaka Nagai NT. Collection and Handling of Blood. In: L.Dacie J.V, editor. Practical haematology. 11th ed. Churchill Livingstone; 2012. p. 1–9.
Olujohungbe A, Hambleton I, Stephens L, Serjeant B, Serjeant G. Red cell antibodies in patients with homozygous sickle cell disease: A comparison of patients in Jamaica and the United Kingdom. Br J Haematol. 2001;113(3):661–5.
Meda E, Magesa PM, Marlow T, Reid C, Robert DJ, Makani J. Red Blood Cell Alloimunisation in Sickle Cell Disease Patients in Tanzania. East African Journal of Public Health. 2014;11 (9):775–80.
Published
Issue
Section
License
Copyright (c) 2024 Nigerian Journal of Haematology

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.