Haemoglobin CO-Arab Mimicking HbSS and HbSC: A Case Report
DOI:
https://doi.org/10.60787/njh.vol8no1.90Keywords:
Haemoglobin CO-Arab, MimicsAbstract
Introduction: Haemoglobin C-O Arab is an infrequent condition with limited literature documentation. The underlying mutations in HbC and HbO-Arab affect positions 6Glu → Lys and 121Glu → Lys of the Beta-globin gene, respectively. Interestingly, when both HbC and HbO-Arab are inherited, the individual has the same mutations (Glu → Lys) at different positions (6 and 121) of the same globin chain. The consequences of these interactions make this a unique and enigmatic condition.
Aim: To report a case of HbCO-Arab mimicking HbSS in a patient.
Method: A case report of the patient’s clinical note.
Results: A 26-year-old Fulani lady presented to the Haematology Day Care (HDC) due to varying Hb electrophoresis results. She gave a history of recurrent headaches, occasional bone pains and easy fatiguability. However, no history of jaundice or blood transfusions. Hb electrophoresis done at 6 years was suggestive of HbSS. No history suggestive of sickle cell complications except for a history of parapneumonic effusions at the age of 21 years. Two of her siblings are said to be patients living with sickle cell disease.
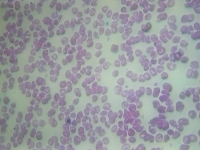
There was no jaundice, pallor, cyanosis or sickle cell habitus. Four previous Hb electrophoreses using alkaline media revealed a single band in the S position except for one, which showed two bands in the S and C regions. A repeat upon presenting to the unit showed a single band at the S region on alkaline electrophoresis. Haematocrit over three years ranged from 32.7% to 40.8%
Given the atypical presentation (history and physical examination) and discrepancies in electrophoresis results, HPLC was done. The presence of an unknown band further added to the diagnostic dilemma. The sample was then sent to the Synnovis Special Haematology Laboratory at Guys and St Thomas Hospital, London, for further testing. Sanger sequencing was performed on the beta-globin genes. This demonstrated compound heterozygous mutations for Hb C due to the HBB;c.19G>A and Hb O-Arab due to the HBB;c.364G>A mutations.
Conclusion: A high index of suspicion and domesticated diagnostic algorithms are needed, especially in resource-constrained settings.
Downloads
References
1.Kohne E. Hemoglobinopathies: clinical manifestations, diagnosis, and treatment. Dtsch Ärztebl Int. 2011 Aug;108(31-32):532-40. doi: 10.3238/arztebl.2011.0532.
2.Williams TN, Weatherall DJ. World distribution, population genetics, and health burden of the hemoglobinopathies. Cold Spring Harb Perspect Med. 2012 Sep 1;2(9):a011692. Doi: 10.1101/cshperspect.a011692.
3.Piel FB, Howes RE, Patil AP, Nyangiri OA, Gething PW, Bhatt S, et al. The distribution of haemoglobin C and its prevalence in newborns in Africa. Sci Rep. 2013;3:1671. doi: 10.1038/srep01671.
4.Usanga EA, Andy JJ, Ekanem AD, Udoh EA, Udoh AE. Haemoglobin C gene in southeastern Nigeria. East Afr Med J. 1996;73(9):566-7.
5.Karna B, Jha SK, Al Zaabi E. Haemoglobin C Disease. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559043/
6.Schaefer BA, Kiyaga C, Howard TA, Ndeezi G, Hernandez AG, Ssewanyana I, et al. Haemoglobin variants identified in the Uganda Sickle Surveillance Study. Blood Adv. 2016 Nov 22;1(1):93-100. doi: 10.1182/bloodadvances.. 2016000950.
7.Elbashir I, Elsayed Yousif TY. Molecular Detection of Haemoglobin O-Arab in the Sudanese Population. Int J Gen Med. 2023;16:3323-30. doi: 10.2147/IJGM.S421140.
8.Joutovsky A, Nardi M. Hemoglobin C and Hemoglobin O-Arab Variants Can Be Diagnosed Using the Bio-Rad Variant II High-Performance Liquid Chromatography System Without Further Confirmatory Tests. Arch Pathol Lab Med. 2004 Apr;128(4):435-9. doi: 10.5858/2004-128-435-HCAHOV.
9.Kini K, Warrier R, Maeda K. Hematological Studies In Hemoglobin So Arab And Co Arab Diseases: Clinical And Laboratory Evaluation. Pediatr Res. 1981;15(Suppl 4):580. doi: 10.1203/00006450-198104001-00850.
10.Maeda K, Kini RK, Saeed SM, Rucknagel DL. Haemoglobin SO Arab and haemoglobin CO Arab diseases. Clinical and laboratory study. Am J Pediatr Hematol Oncol. 1983 Summer;5(2):127-31.
11.Akodu S, Diaku-Akinwumi I, Njokanma O. Age at diagnosis of sickle cell anaemia in Lagos, Nigeria. Mediterr J Hematol Infect Dis. 2013;5(1):e2013001. doi: 10.4084/MJHID.2013.001.
12.Brown BJ, Akinkunmi BF, Fatunde OJ. Age at diagnosis of sickle cell disease in a developing country. Afr J Med Med Sci. 2010;39(3):221-5.
13.Chukwu BF, Ezenwosu OU, Eke CB, Chinawa JM, Ikefuna AN, et al. What Factors Influence the Age at Diagnosis of Sickle Cell Anaemia in Enugu, Nigeria? J Blood Disord Transfus. 2014;5:231. doi: 10.4172/2155-9864.1000231.
14.Claeys A, Van Steijn S, Van Kesteren L, Damen E, Van Den Akker M. Varied Age of First Presentation of Sickle Cell Disease: Case Presentations and Review. Case Rep Med. 2021 Feb 8;2021:8895020. Doi: 10.1155/2021/8895020.
15.Wild BJ, Bain BJ. Investigation of Variant Haemoglobins and Thalassaemias. In: Bain BJ, Bates I, Laffan MA, editors. Dacie and Lewis Practical Haematology. 12th ed. Elsevier; 2017. p. 282-311. doi: 10.1016/B978-0-7020-6696-2.00014-X.
16.Kotila TR. Guidelines for the diagnosis of the haemoglobinopathies in Nigeria. Ann Ib Postgrad Med. 2010;8(1):25-9.
17.LabCE. Hemoglobinopathies: Haemoglobin S Disorders. Available from: https://www.labce.com/spg422877_solubility_test_errors.aspx [Accessed 2025 Feb 12].
18.Old J, Harteveld CL, Traeger-Synodinos J, et al. Prevention of Thalassaemias and Other Haemoglobin Disorders: Volume 2: Laboratory Protocols [Internet]. 2nd ed. Nicosia (Cyprus): Thalassaemia International Federation; 2012. Available from: https://www.ncbi.nlm.nih.gov/books/NBK190579/
19.Bhusal A, Bhandari S, Sah RP. Can HPLC be used as an ideal methodology instead of Hb Electrophoresis for the diagnosis of hemoglobinopathies in a routine clinical laboratory of an under-resourced country like Nepal? Ann Med Surg (Lond). 2022 Aug 18;82:104367. Doi: 10.1016/j.amsu.2022.104367.
20.Traeger-Synodinos J, Harteveld CL, Old JM, Petrou M, Galanello R, Giordano P, et al. EMQN Best Practice Guidelines for molecular and haematology methods for carrier identification and prenatal diagnosis of the haemoglobinopathies. Eur J Hum Genet. 2015;23(4):426-37
Published
Issue
Section
License
Copyright (c) 2025 Nigerian Journal of Haematology

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.