Sickle Cell Disease-Related Complications among a Cohort of Steady State Sickle Cell Anaemia Patients in a Tertiary Hospital, North-Western Nigeria.
DOI:
https://doi.org/10.60787/njh.vol9no1.89Keywords:
Sickle cell disease-related complications, sickle cell anaemia, steady state, North-western NigeriaAbstract
Background: As the survival rate of Sickle Cell Disease (SCD) patients has increased in the last few decades, more patients are presenting with complications of the disease. The pattern and distribution of these complications will determine resource allocation, intervention and prevention strategies.
Aims and Objectives: The study identified and characterised the different SCD-related complications (SDRCs) in a cohort of Sickle Cell Anaemia (SCA) patients in North-western Nigeria.
Materials and Methods: This was a descriptive cross-sectional study in which 100 SCA patients in a steady state were recruited consecutively. Information on socio-demographics and medical history was obtained using case files and interviewer-administered questionnaires. We determined the steady-state haematological and biochemical parameters. The primary outcome was the proportion of the different SDRCs and their laboratory and clinical characteristics.
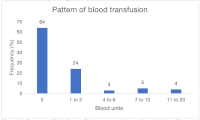
Results: Sickle Cell Anaemia patients (78% females and 22% males) aged between 18 and 43 years were enrolled. The most common SDRCs included avascular necrosis (16%), chronic leg ulcer (14%), stroke (11%), priapism (24.8%), acute chest syndrome (5%), renal disease (4%), and pulmonary hypertension (1%). Bone pain crises (57%) were the main reason for hospital admission. Steady-state haematological parameters were similar across patients, but total bilirubin was significantly higher among those with avascular necrosis (p-0.014), while direct bilirubin was higher in patients with chronic leg ulcer (p-0.001) and priapism (p-0.007). Thirty-six per cent (36%) of the patients had blood transfusions, with patients suffering from renal disease receiving the highest volume (6.75 units per patient).
Conclusion: Findings of this study will guide decision-making among clinicians and policymakers in the management and prevention of SCD-related complications.
Downloads
References
1. Kaushansky K, Lichtman M, Beutler E, Kipps T, Seligsohn U, Prchal J. Disorders of Haemoglobin Structure: Sickle Cell Anaemia and Related Abnormalities. In: Natarajam K, Townes TM KA, editor. Williams Haematology. China: McGraw-Hill; 2010. page 709–34.
2. Odievre M, Verger E, Cristine A, Silva-pinto, J E. Pathophysiological insights in sickle cell disease. Indian J Med Res 2011;134:532–7.
3. Ahmed S, Kagu M, Abjah U, Bukar A. Seasonal Variations in Frequencies of Acute Vaso-Occlusive Morbidities among Sickle Cell Anaemia Patients in Northern Nigeria. J Blood Disord Transfus 2012;3:1–5.
4. Steinberg MH. Fetal hemoglobin in sickle cell anemia. Blood 2020;136(21):2392–400.
5. Jude M, Aliyu G, Nalado A, Garba K, Florence F, Hassan A, et al. Stroke prevalence amongst sickle cell disease patients in Nigeria: a multi-centre study. Afr Heal Sci 2014;14:446–52.
6. Lubeck D, Agodoa I, Bhakta N, Danese M, Pappu K, Howard R, et al. Estimated Life Expectancy and Income of Patients With Sickle Cell Disease Compared With Those Without Sickle Cell Disease. JAMA Netw open 2019;2(11):e1915374.
7. Kato G, Gladwin M, Steinberg M. Deconstructing Sickle cell disease: Reappraisal of the role of haemolysis in the development of Clinical Subphenotypes. Blood 2007;21:37–47.
8. WHO. Management of birth defects and haemoglobin disorders; Report of a joint WHO-march of Dimes meeting. Geneva: World Health Organization. 2006.
9. Demographic Statistical Bulletin 2022. Natl Bur Stat :Accessed;20/12/2024.
10. Chinegwundoh FI, Smith S, Anie KA. Treatments for priapism in boys and men with sickle cell disease. Cochrane database Syst Rev 2017;9(9):CD004198.
11. Adegoke SA, Adeodu OO, Adekile AD. Sickle cell disease clinical phenotypes in children from South-Western, Nigeria. Niger J Clin Pr 2015;8:95–101.
12. Abdulrahman A, Mohammed K, Paula J, Ahmed M, Hazem A, Paola S, et al. Sickle Cell Disease in Saudi Arabia: The Phenotype in Adults with the Arab-Indian Haplotype is not Benign. Br J Haematol 2014;164:597–604.
13. Isa H, Adegoke S, Madu A, Hassan AA, Ohiaeri C, Chianumba R, et al. Sickle cell disease clinical phenotypes in Nigeria: A preliminary analysis of the Sickle Pan Africa Research Consortium Nigeria database. Blood Cells Mol Dis 2020;84:102438.
14. Ambe JP, Mava Y, Chama R, Farouq G, Machoko Y. Clinical Features of Sickle Cell Anaemia in Northern Nigerian Children. West Afr J Med 2012;31(2):81–5.
15. Alsultan A, Aleem A, Ghabbour H, AlGahtani F, Al-shehri A, Elfaki M. Sickle cell disease subphenotypes in patients from southwestern province of Saudi Arabia. Paediatr Hematol Oncol 2012;34:79–84.
16. Madu A, Madu A, Umar G, Ibekwe K, Duru A, Ugwu A. Avascular necrosis in sickle cell (homozygous S) patients: Predictive clinical and laboratory indices. Niger J Clin Pr 2014;17:86–9.
17. Ware H, Brooks A, Toye R, Berney S. Sickle cell disease and silent avascular necrosis of the hip. J Bon Jt surg Br Vol 1991;73:947–9.
18. Adekile A, Gupta R, Yacoub F, Sinan T, AI Bloushi M, Haider M. Avascular necrosis of the hip in children with Sickle cell disease and high haemoglobin F: Magnetic resonance imaging findings and influence of alpha-thalassaemia trait. Acta haematol 2001;105:27–31.
19. Bazuaye G, Nwannadi A, Olayemi E. Leg ulcers in adult sickle cell disease patients in Benin City Nigeria. Gomal J Med Sci 2010;8:190–4.
20. Hassan A, Gayus D, Abdurasheed I, Umar M, Ismail D, Babadoko A. Chronic Leg ulcer in Sickle Cell Disease Patients in Zaria, Nigeria. Arch Int Surg 2014;4:141–5.
21. Clare A, FitzHenley M, Harris J, Hambleton I, GR S. Chronic leg ulceration in homozygous sickle cell disease: the role of venous incompetence. Br J Haematol 2002;119:567–71.
22. Lagunju I, Brown B. Adverse neurological outcomes in Nigerian children with sickle cell disease. Int J Hematol 2012;96:710–8.
23. Galadanci AA, Galadanci NA, Jibir BW, Abdullahi SU, Idris N, Gambo S, et al. Approximately 40 000 children with sickle cell anemia require screening with TCD and treating with hydroxyurea for stroke prevention in three states in northern Nigeria. Am J haematol 2020;94(11):1–5.
24. Ya’u NA, Mustapha FG, Abdulqadir I. Sickle Cell Anaemia (SCA) related priapism in Kano, North- Western, Nigeria; re-emphasizing the important role of haemolysis. J Med Res 2023;9(4):84–7.
25. Adeyoju A, Olujohungbe A, Morris J, Yardumian A, Bareford D, Akenova A. Priapism in sickle cell disease; incidence, risk factors and complications-an international multicentre study. BJU Int 2002;90:898–902.
26. Bolarinwa R, Akinlade K, Kut M, Olawale O, Akinola N. Renal disease in Adult Nigerians with Sickle cell anaemia: A report of prevalence, clinical features and risk factors. Saudi J Kidney Dis Transpl 2012;23:171–5.
27. Richard K, Derick Nii M, Obed C, Enos A, Lyudmila A, Juliana M, et al. Chronic kidney disease is common in sickle cell disease: a cross-sectional study in the Tema Metropolis, Ghana. BMC Nephrol 2015;16:75.
28. Platt O, Brambilla D, Rosse W, Milner P, O C. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med 1994;330:1639–44.
29. Zakari Y, Gordenk V, Sachdev V, Babadoko A, Mamman A, Akpanpe P. Prevalence and risk factors for pulmonary artery systolic hypertension among sickle cell disease patients in Nigeria. Am J haematol 2008;83:450–90.
30. Ataga KI, Moore CG, Jones S et al. Pulmonary hypertension in patients with sickle cell disease: A longitudinal study. Br J Haematol 2006;134:109–115.
31. Nelson SC, Adade BB, McDonough EA et al. High prevalence of pulmonary hypertension in children with sickle cell disease. J Pediatr Hematol Oncol 2007;29:334–337.
Published
Issue
Section
License
Copyright (c) 2025 Nigerian Journal of Haematology

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.